Bhattacharya Lab (Lung Biology Lab)
Location and Contact Information
- Office 212-305-7310
- Lab 212-305-6724
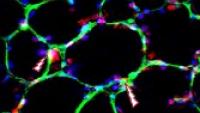
The Lung Biology Laboratory specializes in single- and two-photon laser scanning microscopy of the intact lung. The overall direction is to apply real-time imaging in understanding molecular mechanisms underlying acute lung injury (ALI) and ARDS. ALI results from breakdown of the air-blood barrier. The resulting respiratory failure requires respiratory support by mechanical ventilators in critical care units. It is estimated that about 250,000 people suffer from ALI in the US alone. The mortality rate is >30%. Patients who survive the disease continue to have long-term morbidity. Despite these statistics, there is really no "cure" for ALI in the sense that one cannot administer an agent that reverses the illness or blocks its progress. The available therapy continues to be supportive through ventilator and fluid therapy.
Prime causes of ALI are infection and sepsis. According to the WHO, lower respiratory tract infections are the fifth largest cause of death in high-income countries and the third largest cause worldwide. During the pandemic, COVID emerged as a major cause of ALI/ARDS. Other causes include gastric acid aspiration, lung barotrauma, pulmonary embolism, and smoke inhalation. These conditions can be replicated in animal models, providing a means to understand basic disease mechanisms and to develop products that might be therapeutically effective in the clinical setting.
Our ongoing projects include research in immunity, fluid barriers, barrier-enhancing biologics (we have patented one biologic), surfactant secretion, water secretion, micromechanics, stem cells and macrophages. In the last three years, our publications have appeared in high-impact journals, including the Journal of Clinical Investigation, Nature Communications, Nature Medicine and Nature.
Select Publications
Galina A. Gusarova, Shonit R. Das, Mohammad N. Islam, Kristin Westphalen, Guangchun Jin, Igor O. Shmarakov, Li Li, Sunita Bhattacharya, Jahar Bhattacharya; Actin fence therapy with exogenous V12Rac1 protects against Acute Lung Injury. JCI Insight. 2021 Mar 22; 6(6): e135753. PMCID: PMC8026177
Jasmine Lee*, Mohammad Naimul Islam*, Kaveh Boostanpour, Dvir Aran, Stephanie, Christenson, Michael A. Matthay, Walter Eckalbar, Daryle J. DePianto, Joseph R., Arron, Liam Magee, Sunita Bhattacharya, Rei Matsumoto, Masaru Kubota, Donna L. Farber, Jahar Bhattacharya*, Paul J. Wolters*, Mallar Bhattacharya*. *Equal contribution. Molecular programs of fibrotic change in aging human lung. BioRxiv preprint, January 19, 2021. (Accepted by Nature Communications).
Hough RF, Islam MN, Gusarova GA, Jin G, Das S, Bhattacharya J. (2019). Endothelial mitochondria determine rapid barrier failure in chemical lung injury. JCI Insight 4(3). PMID:30728333
Hook JL, Islam MN, Parker D, Prince AS, Bhattacharya S, Bhattacharya J. Disruption of staphylococcal aggregation protects against lethal lung injury. J Clin Invest. 2018; 128 (3): 1074-1086. PMID: 29431734.
Westphalen K. Gusarova G, Islam MN, Subramanian M, Cohen TS, Prince AS, Bhattacharya J. (2014). Sessile alveolar macrophages modulate immunity through connexin 43-based epithelial communication. Nature 2014. 506:503-6. PMID:24463523
Islam MN, Das SR, Emin MT, Wei M, L Sun, Westphalen K, Rowlands D, Quadri S, Bhattacharya S, Bhattacharya J. Mitochondrial transfer from bone marrow-derived mesenchymal stromal cells to pulmonary alveoli protects against acute lung injury. Nat Med. 2012. 18:759-765. PMID:22504485
Quadri S, Sun L, Islam MN, Shapiro L, Bhattacharya J. Cadherin selectivity filter regulates endothelial sieving properties. Nat Commun. 2012; 3:1099. PMID:23033075