Infectious Diseases
|
Application Deadline |
November 1 |
|
Length of Program |
3 years |
|
Program Start Date |
July 7 |
|
Number of Positions Available |
Usually 1 per year |
The goal of our fellowship program is to provide optimal training for pediatricians who want to become board-certified specialists in pediatric infectious diseases and pursue careers in academic and/or hospital-based practice. We offer a curriculum tailored to the individual interests of our trainees, including concentration tracks within antimicrobial stewardship, infection prevention and hospital epidemiology, and immunocompromised host. A central focus of our training program is the selection of a strong mentor for each of our trainees to assure their optimal development and future success. We value diversity, equity, and inclusion, and maintain a rich academic environment where mentors and trainees of diverse backgrounds come together to advance children’s health.
Clinical Service
Inpatient clinical service consists of 12 months total over a three-year period spent at the NewYork-Presbyterian Morgan Stanley Children's Hospital, within Columbia University Irving Medical Center in New York City’s diverse Washington Heights neighborhood. This hospital, originally founded in 1887 as Babies Hospital, has a rich history of contributions to pediatric clinical care and research, and a strong focus on quality improvement and advocacy, which continues to this day.
Morgan Stanley Children's Hospital is the top-top-ranked children’s hospital in the New York metropolitan area, in the 2023-2024 U.S. News & World Report rankings, and offers care to patients across wide range of clinical subspecialties. The hospital houses more than 250 inpatient beds across various levels of acuity and is a Level 1 pediatric trauma center, a Level 1 ACS Level I Children's Surgery Center, and the only platinum-designated ECMO Center in New York. It is home to top tier bone marrow and solid organ transplantation programs, in addition to an active primary immunodeficiency clinic. The breadth and diversity of clinical exposure here is unparalleled, and ensures that our graduates are ready for independent clinical practice in a wide range of pediatric infectious diseases settings and roles.
In addition to inpatient service, fellows maintain an active longitudinal presence in our ambulatory clinic settings (in-person and telehealth) including within general infectious diseases, post-surgical infections, immunocompromised hosts, and HIV/STIs, with additional opportunities available to work in immunology, adult HIV, adult immunocompromised host clinics. We have a dedicated PharmD on staff, who rounds with our team daily, and a support infrastructure that ensures seamless transitions of care. Various learners interface with our team, including rotating medical students, residents, pharmacy students, hospitalist fellows, and ensures a robust learning environment.
Research and Education
The Department of Pediatrics receives over $25 million in sponsored research funding, and is first in the Northeast per the Blue Ridge NIH Ranking for Pediatrics, and the Division of Infectious Diseases has a long track record of training independent investigators in clinical and basic science research. The division's research activities reflect the broad scope of infectious diseases and range from global and local epidemiological studies, to analysis of microbial communities and evolution, bacterial and viral pathogenesis, testing and safety issues, as well as clinical trials.
Division members are very closely associated with the research activities of Columbia University. We contribute to and take full advantage of the outstanding research community here, benefiting from the many collaborative centers that support our technical capabilities, including the Irving Institute, and we provide a forum for innumerable seminars and colloquia in related areas of basic and translational research.
Fellows can participate in our NIH-funded T32 training grant research activities, with a broad range of projects available in basic/translational science, epidemiology, and bioinformatics. These projects, mentored by NIH-funded faculty from Columbia University and Weill Cornell Medical College, encompass a wide array of research areas including host susceptibility to infection, immunogenetics and immunity, to infection in neonates and early childhood.
In addition, our fellows and faculty pride themselves on a strong commitment to teaching, both at the bedside and in formal didactics. Division members are involved in teaching at all levels, from basic infectious pathophysiology in the preclinical medical student curriculum, to teaching clinical application of infectious diseases concepts to medical students in pediatric clerkship and pediatric residents and fellows.
Fellows participate in a variety of didactic programs:
- Pediatric ID rounds (once weekly)
- Joint Pediatric-Adult ID rounds (twice weekly)
- Micro rounds (once weekly)
- Joint Pediatric-Adult ID fellow boot camp (mornings in July)
- A variety of journal club and research presentations.
Fellows also formally rotate within microbiology, antimicrobial stewardship, and hospital epidemiology, and can pursue external rotations at local hospitals or the NYC Department of Health. Trainees are also encouraged to pursue formal training at the Graduate School of Arts and Sciences or at the Mailman School of Public Health with recent past trainees having earned MS and MPH degrees in public health and bioinformatics.
Antimicrobial Stewardship and Infection Prevention
Our program has always maintained a strong focus on infection prevention and control and antimicrobial stewardship, with an increasing focus on diagnostic stewardship. We have a dedicated fellowship training curriculum in these domains, given how critical these areas are to infectious diseases practice across the spectrum of healthcare settings. All fellows are actively involved in both programs and can choose further concentration depending on their future career goals. Our multidisciplinary Infection Prevention and Control and Hospital Epidemiology team, led by Dr. Lisa Saiman, features a dedicated staff of infectious preventionists devoted to pediatrics, data analysts, and administrative support personnel. Our Antimicrobial Stewardship Program has a dedicated antimicrobial physician steward and a infectious diseases pharmacist, supported by a strong informatics team to provide robust outcomes and data-driven practice modulation. Our fellows have a long track record of academic scholarship and research in these areas with numerous past trainees now occupying leadership roles within IP&C and stewardship.
Pediatric Immunocompromised Host Service
A major emerging focus of our infectious diseases program, the Pediatric Immunocompromised Host (PICH) service, addresses the challenge of infection in the immunocompromised host, including those with a history of malignancy, primary immunodeficiency, immunomodulatory therapy, or following solid or bone marrow transplantation. For such patients, we establish longitudinal care across both the inpatient and outpatient settings, beginning prior to transplant, and following through transplantation and beyond. Our fellows actively engage in the PICH service at all levels, with additional opportunities arising as we develop a dedicated post-graduate fellowship training program in the care of the immunocompromised host.
Infectious Diseases Elective for Students and Residents
As a division, we strongly value teaching and education, and welcome learners at all levels to join us on the wards. This includes medical students and residents at Columbia, as well as visiting trainees.
Medical students at VP&S medical students should enroll in the elective via the VP&S clerkship enrollment form. Medical students from outside institutions should contact the VP&S registrar's office for guidance on scheduling a visiting clerkship.
Pediatric residents at Columbia should enroll via elective enrollment through the Pediatric Chief Residents. Pediatric residents from outside institutions should contact our program coordinator, Julia Zhou (jz78@cumc.columbia.edu) for further details.
Benefits
Residents are employees of NewYork-Presbyterian Hospital and affiliated with Columbia University Irving Medical Center. With these affiliations come many benefits!
How to Apply
Applications to our fellowship are processed through the Electronic Residency Application Service (ERAS) system. Materials are accepted starting in July for fellowship positions beginning the following year. For applicants planning for a July 2021 start date, interviews for all pediatric infectious diseases fellowships at US centers will only be offered virtually in compliance with the guidelines of the Pediatric Infectious Disease Society. This is to ensure that the recruitment process is fair, equitable, and socially responsible. Those who wish to apply must be board eligible or board certified in general pediatrics by the American Board of Pediatrics. Please note that a completed application includes:
- Completed ERAS forms
- Three letters of recommendation, including one letter from the applicant's department chairman or residency director
- Curriculum vitae
- Personal statement
- Additional information, such as USMLE transcript and photo, are recommended
Acceptances to the fellowship are made through the Pediatric Specialties Fall Match of the National Residency Matching Program (NRMP). Please refer to the NRMP website for details about the match submission deadline.
Columbia University and NewYork-Presbyterian Hospital are equal opportunity employers; applications from women and minorities are encouraged. Please note that Columbia University and NewYork-Presbyterian Hospital do not sponsor H1B visa trainees.
Contact
Natalie Neu, MD
nn45@cumc.columbia.edu
Current Fellows
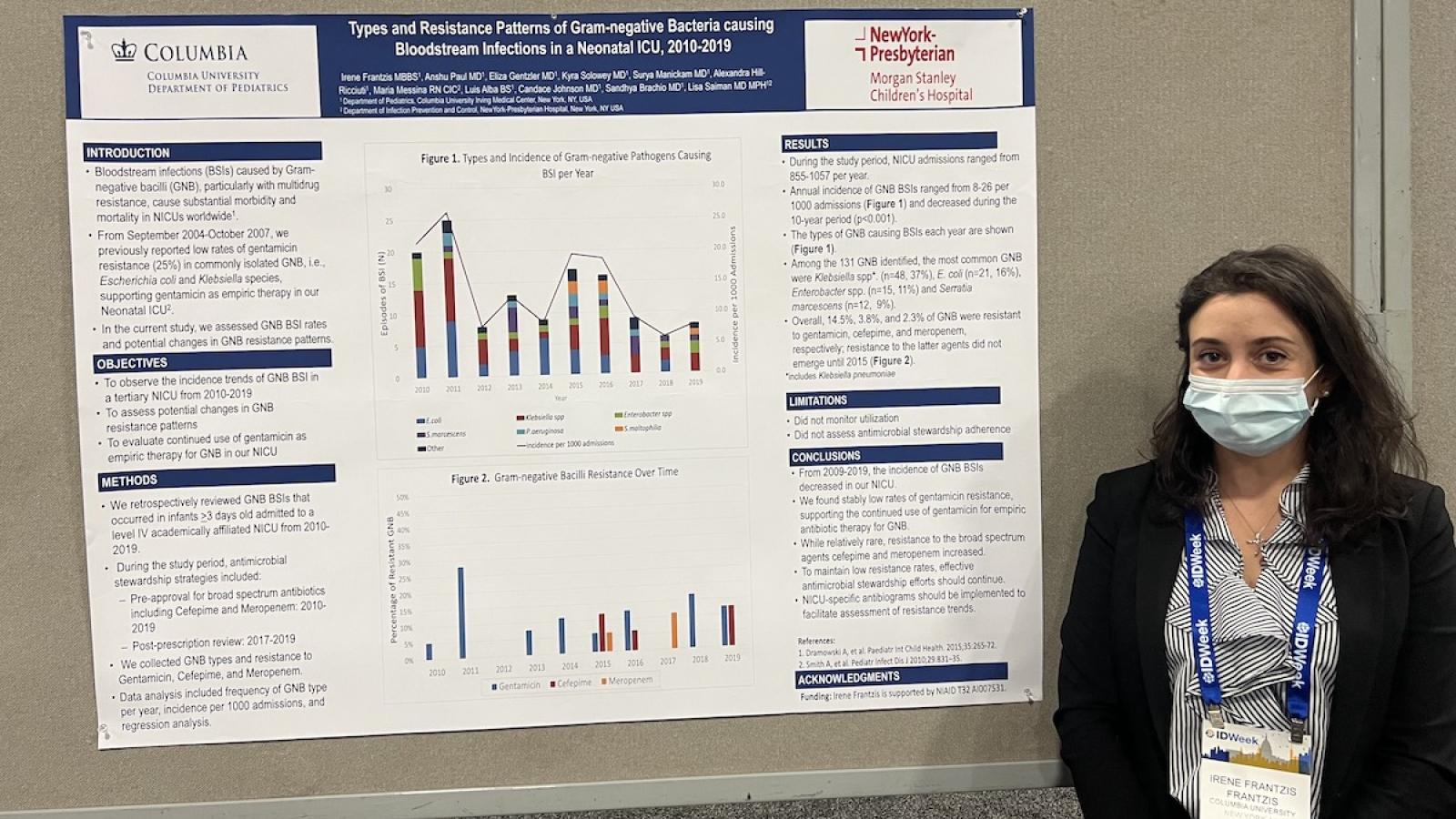
Irene Frantzis, MBBS, MSc
Medical School: St. George's Hospital, University of London
Residency: Einstein Medical Center Philadelphia
Research Interest: Global Infection Prevention & Control, Diagnostic Stewardship
Favorite Bug/Drug: Brucella (still hoping to isolate it!)
Favorite NYC spot: Cote (Michelin-rated Korean BBQ), Elea (Greek comfort food)
Samiksha Tarun, MD, MS
Medical School: Saint Louis University
Residency: University of Michigan
Research Interest: Global Health
Favorite Bug/Drug: MRSA and Meropenem
Favorite NYC spot: Running along the Hudson!
Itay Berger, MD
Medical School: Joyce & Irving Goldman Medical School, Ben-Gurion University of the Negev
Residency: Schneider Children's Medical Center of Israel
Research Interest: Transplant Infectious Diseases
Favorite Bug/Drug: Drainmycin
Favorite NYC spot: Central Park
Graduates of the Fellowship Program
Our fellows have gone on to be diverse roles within the pediatric infectious diseases research and clinical community, serving as leaders and mentors within academia and industry, as well as national and regional advisory boards.
- Valerie Waters, Professor, University of Toronto, Canada
- Kristina Feja, Division Chief, St. Peter’s University Hospital, NJ
- Ouzama Nicholson, Vice President Clinical Development, Dynavax Technologies
- David Michalik, Associate Clinical Professor, University of California Irvine School of Medicine, CA
- Sameer Patel, Associate Professor of Pediatrics, Northwestern University, IL
- Catherine Yen, Clinical and Public Health Coordinator, International Organization for Migration, Washington, DC
- Paul Planet, Assistant Professor, University of Pennsylvania, PA
- Karina Top, Associate Professor of Pediatrics, Dalhousie University, Halifax, Canada
- Saul Hymes, Associate Professor of Pediatrics, Albany Medical Center, NY
- Christina Gagliardo, Assistant Professor, Thomas Jefferson University; attending physician at Atlantic Health System, NJ
- Sruti Nadimpalli, Associate Clinical Professor, Stanford University, CA
- Philip Zachariah, Associate Director Vaccine Research, Pfizer, Inc.
- Jennifer Duchon, Associate Professor in Newborn Medicine, Mt. Sinai, NY
- Candace Johnson, Assistant Professor of Pediatrics, Columbia University Irving Medical Center, NY
- Karen Acker, Assistant Professor of Pediatrics, Weill Cornell Medical School, NY
- Jason Zucker, Assistant Professor of Medicine and Pediatrics, Columbia University Irving Medical Center, NY
- Shivang Shah, Assistant Professor of Pediatrics, Columbia University Irving Medical Center, NY
- Katia Halabi, Assistant Professor of Pediatrics, Nationwide Children's Hospital, OH
- Irene Frantzis, Assistant Professor of Pediatrics, Columbia University Irving Medical Center, NY