Columbia University
Irving Medical Center
Neurological Institute
710 West 168th Street, 3rd floor
(212) 305-1818
Featured Research
7th ANNUAL TAUB RETREAT
October 2016
Introduction to Columbia Technology Ventures
Ron Katz, PhD, MBA, Senior Technology Licensing Officer and Associate Director of Columbia Technology Ventures (CTV) on the Manhattanville campus, opened up the retreat with an introduction to CTV, the technology transfer office, which facilitates the transfer of inventions from academic research labs to the market for the benefit of society. According to Dr. Katz, each year, CTV manages more than 350 invention disclosures and 100 license deals, involving over 750 inventors across Columbia's campuses. Dr. Katz spoke with Taub's faculty about protecting their intellectual property, describing how certain activities "may diminish chances of obtaining a patent, including disclosure of your invention during presentations, as well as publishing research." Dr. Katz strongly encouraged potential inventors to "get in touch with CTV as early as possible in the innovation process" to patent their technology. He described how CTV, as a leader in university technology transfer, is consistently one of the most successful institutions in terms of revenue generated, as well as the number of licenses, options, and startup companies formed each year. In closing, Dr. Katz detailed how inventors/researchers and their labs, schools, departments, and the University all share in any licensing revenue, distributed in accordance with the Intellectual Property Policy in the University's Faculty Handbook.
For more information, please email Ron Katz, PhD, MBA ron.katz@columbia.edu.
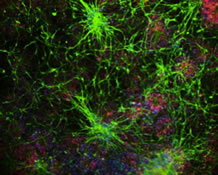
Propagation of Pathology: Mechanisms and Therapeutic Opportunities
Dr. Karen Duff reviewed current research from her laboratory on the mechanisms by which tauopathy could propagate between brain cells, leading to progressive worsening of tau pathology in Alzheimer's disease (AD). Dr. Duff described how, "in the aged EC (entorhinal cortex)-tau mouse model, the spread of tau pathology from hippocampal formation to the neocortex is accompanied by overt cell loss and cognitive impairment." According to Dr. Duff, this mouse model represents the earliest stages of tauopathy and cognitive decline seen in AD. She hypothesized that "triggers of tauopathy may include hyper excitability mediated by APP metabolites." The Duff laboratory has shown that one way by which tau can accumulate in cells is due to dysfunction of proteasome mediated clearance mechanisms, and they have demonstrated that possible therapeutic pathways, aimed at enhancing proteasome activity (PKA activation), may be effective against early stage tauopathy. Most recently, Dr. Duff and team have been investigating how the activation of such clearance pathways by a range of drugs may be effective against tauopathy spread, in vitro and in vivo.
For more information, please email Karen Duff, PhD, ked2115@columbia.edu.
Harnessing Hypoxic Adaptation to Treat Neurological Disorders
Next, Rajiv Ratan, MD, PhD, Burke Professor of Neurology and Neuroscience; Associate Dean, Weill Medical College; and Executive Director, Burke Medical Research Institute, a focus of his work as director of the Laboratory for Redox Biology and Neural Protection and Repair at Burke. According to Dr. Ratan, "since its inception in 1994, the laboratory has utilized an in vitro model of oxidative stress to understand the precise mechanisms by which disrupted redox homeostasis leads to death in neurons. This simple model system, which harnesses the experimental leverage of primary neurons in cell culture, has spawned a large number of exciting projects in the lab and projects targeted by progeny of the lab." Dr. Ratan has long hypothesized that "disease is a failure of compensation," and has sought "better understanding of how the nervous system adapts to injury with a particular focus on epigenetic modulators (HDACs, transglutaminase, MecP2) and transcription factors (Sp1, CREB, HIF-1alpha), as well as enzymes that modulate the stability of these factors (HIF prolyl hydroxylases)."
For more information, please email Rajiv Ratan, MD, PhD, rrr2001@med.cornell.edu.
Early Phase Adaptive Trials: A Gateway from Mice to Humans
Following the morning break, Dr. Ying Kuen (Ken) Cheung, Professor of Biostatistics from the Mailman School of Public Health, spoke about the benefits of adaptive study designs versus conventional statistical designs in early phase clinical trials. According to Dr. Cheung, "an adaptive clinical trial is a study that includes a prospectively planned opportunity for adaptations of the study design and hypotheses based on interim analysis of the study data." Such adaptations, he explained, are useful learning tools in early phase trials by maximizing relevant information in the trial data, and can be a means of bridging the knowledge gap between preclinical and clinical phase for the purposes of treatment screening and dose ranging. Dr. Cheung gave an example of the continual reassessment method, an adaptive dose finding design, which would require fewer patients than a randomized design to achieve the same accuracy in terms of identifying the maximum tolerated dose, and would overdose fewer study participants. Dr. Cheung also acknowledged the promise of efficiency could come with a "cost" in the short term. "In order to improve the likelihood of a successful phase III confirmatory trial, we may need to design a bigger adaptive early phase trial in order to define the dose, the patient population, and the endpoint more precisely," he said. The advantages of adaptive designs are, in Dr. Cheung’s opinion, "best realized when we take a long-term view."
For more information, please email Ying-Kuen (Ken) Cheung, PhD, yc632@cumc.columbia.edu.
Panel Discussion: Challenges in Clinical Trials and Observational Studies
in at Risk Individuals
Moderator: Karen Marder, MD, MPH
Following Dr. Cheung, a multidisciplinary panel of Taub faculty and staff discussed "Challenges in Clinical Trials and Observational Studies." According to Dr. Karen Marder, co-host of this year's retreat and moderator of this panel discussion, "the goal was to explore the ethical and logistic challenges for participants and staff conducting research in individuals who are at risk for genetic diseases, or who are identified as at risk based on imaging studies. As we are pushing diagnoses earlier and earlier, and offering treatment to individuals who may have few if any symptoms, this presents unique issues." The panel included Dr. Ted Huey, who runs the Taub's FTD program and also serves as the neuropsychiatrist in the Huntington's Disease Center of Excellence at Columbia; Dr. Chuck Kreisl, who spoke about identifying individuals at risk for AD and the identification of tauopathies using novel PET radioligands; Dr. Jennifer Manly, who has been awarded a new family study for children of WHICAP participants and who spoke about study challenges in multiethnic communities, potentially with low education; Jill Goldman, who does genetic counseling in FTD, AD, and HD; and Senior Staff Associate Helen Mejia Santana, who has coordinated studies in families at risk for early onset PD, and currently coordinates the Michael J. Fox Foundation's LRRK2 PPMI study. Together, these panelists covered topics of concern in patient populations across a range of neurodegenerative disorders, including Alzheimer's disease (AD), mild cognitive impairment (MCI), Parkinson's disease (PD), frontotemporal dementia (FTD), and Huntington's disease (HD).
For more information, please email Karen Marder, MD, MPH, ksm1@cumc.columbia.edu.
Genetics and Drug Discovery (Keynote Speaker)
Tim J.R. Harris, PhD, Molecular Biologist and Biochemist, Venture Partner with SV Life Sciences, followed the panel discussion with a dynamic presentation on translational research applicable to these and other disease populations. He described his "data intensive vision for [the future] of patient care," and the ways in which genetics and genomics are driving drug discovery. While oncology currently leads the way, Dr. Harris said, "the same principles apply to neurological diseases such as ALS, PD, AD, and MS." He explained, "molecular pathology is being unraveled by using information derived from the genes known to be involved in the diseases," and added that "multiple drug modalities may be needed to make the most of these discoveries," including monoclonal antibodies, small molecules, anti-sense oligonucleotides, and gene therapy. Dr. Andy Teich, co-host of this year's event said, "keynote speaker Tim Harris was particularly well received…he discussed his recent work studying the role of autophagy in neurodegenerative disease. He also discussed his extensive experience in the biotech industry, including his time at Biogen." Dr. Teich added that Dr. Harris had "encouraged members of the Taub Institute to contact him regarding how we can translate our own work into pre-clinical development."
For more information, please email Tim J.R. Harris, PhD, timothy.harris@svlsa.com.
A Pharmacogenomics Approach for Targeting Negative Symptoms Across Neuropsychiatric Disorders
Following lunch and our Taub Institute Retreat Poster Session, Dr. Catherine Clelland talked about her most recent work targeting negative symptoms across neuropsychiatric disorders. Such symptoms, which include social withdrawal and emotional unresponsiveness, are among the most persistent and debilitating, and contribute significantly to the huge personal and economic costs of severe neuropsychiatric illnesses. According to Dr. Clelland, proline is a precursor of the neurotransmitter glutamate and likely functions as a modulator of CNS neurotransmission. Her laboratory recently found that "the severity of negative symptoms exhibited by patients with schizophrenia were associated with their levels of blood proline along with their genotype of a functional variant in the catechol-O-methyltransferase (COMT) gene: For those with one or two copies of the COMT "Met" allele, having high levels of plasma proline was associated with significantly more negative symptoms or greater symptom severity. Conversely, for patients with two copies of the "Val" allele, high plasma proline levels were associated with significantly less negative symptoms." Dr. Clelland noted that these findings have clinical relevance because they support personalization of negative symptom treatment based upon a patient's COMT genotype, for the purpose of up-, or down-regulating proline levels. Importantly, she added, medications that regulate proline levels already exist, such as the widely used mood stabilizer, valproate. Thus, according to Dr. Clelland, "while longitudinal studies are still needed, our study has implications for therapeutic decisions, for example, specific targeting of valproate treatment to those patients who may benefit (Val/Val patients), and avoiding prescription of valproate for those patients exhibiting negative symptoms who have at least one copy of the COMT Met allele."
For more information, please email Catherine Clelland, PhD, cc2786@columbia.edu.
Heterogeneity of Alzheimer's disease: Implications for Diagnosis,
Prognosis and Clinical Trials Design
Dr. Giuseppe Tosto's talk focused on the fact that, while Alzheimer's disease (AD) most commonly presents in later life as an amnestic syndrome, with impairment in other domains emerging as the disease progresses, variations in cognitive profile, age at onset, rate of decline, and behavioral and motor impairments exemplify the heterogeneity of the disease. For example, explained Dr. Tosto, "when motor signs, behavioral disturbances, or a predominant frontal impairment are present in early stages of the disease, the progression is usually more aggressive. This phenotypic heterogeneity is mirrored by diverse profiles in terms of neuroimaging, biomarkers, and neuropathological findings." Knowledge of AD syndromic heterogeneity is of critical importance to prevention and treatment, explained Dr. Tosto. Current clinical trials usually target specific aspects of the disease, he added, "which might be mixed with other pathological features or be inadequate for atypical subtypes not considered in their inclusion/exclusion criteria."
For more information, please email Giuseppe Tosto, MD, PhD, gt2260@columbia.edu.
Development of Therapeutics Targeting Autophagy and Protein Clearance
Dr. W. Haung (Ho) Yu's presentation focused on a research program that examines protein clearance in Alzheimer's and related disorders. The strategy for his laboratory's research, he explained, is to "identify small molecules that can be used in the treatment of proteinopathies, a pathology common to all neurodegenerative diseases." According to Dr. Yu, this program involves partnerships with NIH/NCATS and the medicinal chemistry group of Dr. Donald Landry (Department of Medicine). Dr. Yu explained, "we are using a systematic approach to validate these small molecules, from pharmacological evaluation (including designing molecules that are brain penetrant) to removal of tauopathies and identification of drug targets related to autophagy." This strategy, he added, "covers work from chemical composition to proof-of-concept studies in cell and in vivo. Our work has identified several small molecules that promote a process called autophagic flux, which includes the development of the autophagic vacuole (AV—here, Dr. Yu notably recognized the work of Dr. Ohsumi, awarded the 2016 Nobel Prize in Medicine), envelopment of proteotoxic aggregates (like tau and α-synuclein), and delivery to and degradation by the lysosome. Our molecules," said Dr. Yu, "work to help clear out the backlog of AVs that accumulate in neurons with aging and neurodegeneration and facilitate the process of removing protein aggregates." Currently, Dr. Yu's lab is at the stage of systematically identifying the best small molecules to take forward into pre-IND testing and, ultimately, for filing for human use with assistance from Columbia Tech Venture and the Columbia Clinical Trials Office.
For more information, please email W. Haung (Ho) Yu, PhD, why2102@cumc.columbia.edu.
Transmitted Electroencephalogram Activity Monitoring (TEAM) Helmet:
A Neurological/Biomedical Engineering Partnership
Dr. James Noble spoke of his participation in the Transmitted Electroencephalogram Activity Monitoring (TEAM) Helmet Project, part of a neurological/biomedical engineering partnership through the Columbia Coulter Program, which provides funding and support for the development of promising biomedical technologies. Dr. Noble described how, through the Coulter Program, awards are provided to multidisciplinary teams to perform specific tasks needed to validate a commercial hypothesis (vs. a scientific hypothesis). Dr. Noble noted how support for the "commercialization of science, not scientific discovery" is a "somewhat novel concept within the university setting." He described his involvement with the project as "an essential step in helping enable [his] vision of creating novel strategies to better diagnose concussion objectively and in real time," adding that he "anticipates the collaborative network [he] developed through the process will benefit [his] professional goals in a sustained and meaningful way."
For more information, please email James Noble, MD, MS, jn2054@columbia.edu.
Dietary Flavanols and Cognitive Aging
Drs. Adam M. Brickman, Frank A. Provenzano, and Dr. Scott Small presented their research on "Dietary Flavanols and Cognitive Aging." Research across species, Dr. Brickman explained, has "demonstrated that the hippocampal formation comprises cellular compartments that mediate distinct behaviors and are differentially implicated in diseases across the lifespan." The dentate gyrus is a region of the hippocampal formation that has been linked to normal age-related memory decline. Dr. Provenzano described their development of neuroimaging tools designed to investigate the aging dentate gyrus and neuropsychological instruments that can distinguish dentate gyrus functioning from other hippocampal subfields. Guided by previous animal studies, Drs. Brickman, Provenzano, and Small showed "experimentally that individuals consuming high cocoa flavanol diets had increased dentate gyrus functioning and improvement on a memory test mediated by the dentate gyrus." Currently, they are conducting two clinical trials that "will formally test the extent to which dietary flavanol consumption can treat normal age-related memory decline." One study, Dr. Brickman explained, "involves in-person assessments and neuroimaging among 250 older adults. The second will be conducted remotely among 4,000 older adults via innovative methods and internet-based cognitive assessments."
For more information, please email Adam Brickman, PhD, amb2139@columbia.edu.