Columbia Center for Translational Immunology

Columbia Center for Translational Immunology (CCTI)
The Columbia Center for Translational Immunology (CCTI) at Columbia University Irving Medical Center is a multi-departmental, multidisciplinary research center aimed at optimizing translation of advances in basic immunology from the laboratory to the clinic, understanding immunological diseases and events in humans and optimizing transfer of information and methodologies to achieve synergy between different disciplines of applied immunology.
CCTI Cores
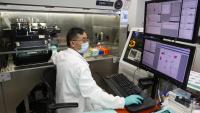
Core facilities within the CCTI include flow cytometry and clinical studies.
News
- April 22, 2024
Established in 2020, the Nelson Awards support basic and translational research in transplantation.
Topic
Transplantation - April 11, 2024
David H. Sachs is Professor of Surgical Sciences (in Surgery) at Columbia Irving Medical Center.
Topic
Campus News - January 19, 2024
Dr. Matthew Yousefzadeh Receives received pilot award and named Trainee Advocate.
Topic
Aging - December 8, 2023
The U.S. Food and Drug Administration is expected to approve exa-cel gene-editing treatment for sickle cell disease. .
Topic
Campus News - September 19, 2023
The CCTI has three recipients of the 2023 Nelson Family Transplant Innovation Awards Program’s Faculty Development Awards.
Topic
Campus News






